CD4+ T cells have been highlighted in the scientific literature for the important role they play in the immune response to lung infections. However, an article published in the journal Cell Reports shows that an imbalance in the volumes of these defense cells in different parts of the lung in response to infection can do more harm than good.
The study described in the article involved infecting mice with hypervirulent tuberculosis and influenza. The authors concluded that an “ideal amount” of CD4+ T cells in the lungs was required for a cure. This finding opens up perspectives for therapeutic interventions aimed at combating diseases that attack the lungs, while not affecting the ability of the adaptive immune system to fight off infection. Even relatively small numbers of CD4+ T cells in the lungs proved sufficient to afford protection against tuberculosis, for example.
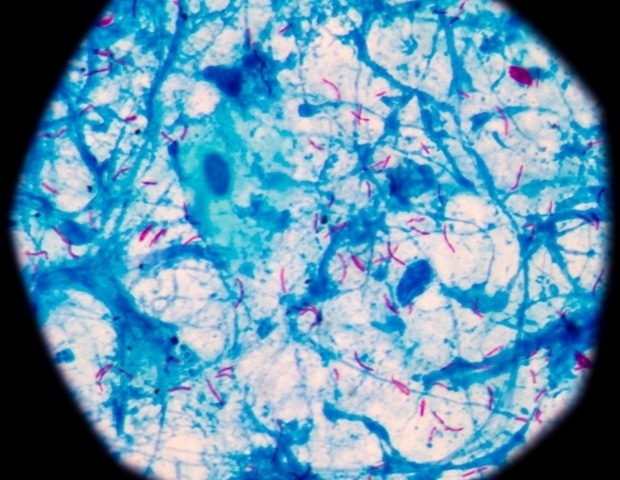
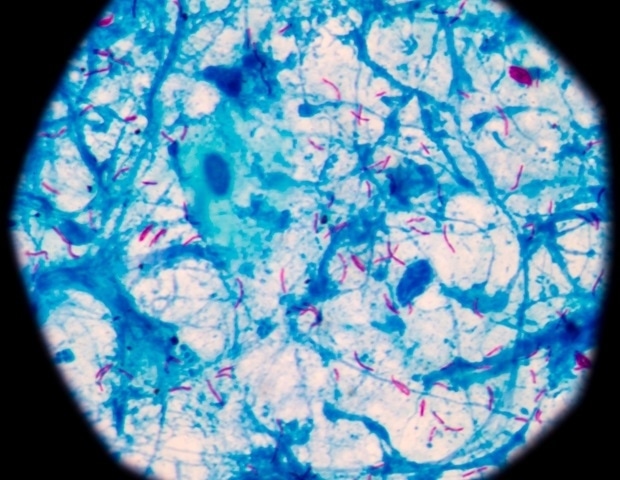
The researchers found that amounts of these cells in lung tissue are mediated by a specific receptor called P2RX7, a protein primarily expressed in immune cells and capable of detecting the presence of extracellular adenosine triphosphate (ATP). The main functions of ATP relate to energy production for cells, but in response to stress or tissue damage it may be released into the external medium, acting as a danger signal for defense cells and potentially leading to an exacerbated response.
In such cases, P2RX7 induces an excessive buildup of CD4+ T cells and boosts expression of the chemokine receptor CXCR3 (chemokines are proteins that direct the migration of white blood cells to infected or damaged tissue). According to the article, the excessive buildup of CD4+ T cells in the mice’s lungs induced by activation of P2RX7 correlated with an increase in the severity of the disease and a reduced survival rate.
ATP in the extracellular medium is recognized by the immune system as a sign of damage because it should be inside the cell rather than outside. Previous research showed how important it is to the development of severe forms of tuberculosis, but the mechanisms weren’t understood. In particular, we didn’t know which type of cell expressed it most. This was what we set out to investigate. We also wanted to find a way to improve the response of these T cells. What we didn’t expect was that removing the receptor to block recognition of ATP would lead to an improvement and not a deterioration.”
Igor Santiago-Carvalho, first author of the article
He has a PhD in immunology and is a researcher at the University of São Paulo’s Biomedical Sciences Institute (ICB-USP) in Brazil.
Santiago-Carvalho’s work was supervised by Maria Regina D’Império Lima, first author of the article and a professor at ICB-USP. She has been researching cellular immunology for 20 years, mainly in malaria, Chagas disease and tuberculosis.
“The more we know about the factors that determine whether the immune response is deficient, optimal or excessive, the better we’ll be able to manipulate it with drugs and treatments to control and even cure the disease,” Lima said.
T cells, or T lymphocytes, are key players in the immune response, which they stimulate and regulate. “For this reason, we wanted to find out which signaling pathways influence immune response optimality. We realized during the project that when tissue is badly damaged, it releases a large amount of damage signals,” she explained. “We were particularly concerned with ATP, and we found that the inflammatory response is intense and harmful when an excessive amount of T cells enter the tissue as they detect ATP. In some cases, it results in pulmonary fibrosis. Intervening in this signaling pathway could be an effective way to reduce the damage done by an excessive immune response to infection.”
The study was supported by FAPESP via a Thematic Project grant awarded to Lima and a direct doctorate scholarship awarded to Santiago-Carvalho.
TB is still a major public health problem worldwide
Tuberculosis is still considered one of the world’s major public health problems, now aggravated by the emergence of drug-resistant bacteria. It is a communicable infectious disease that mainly affects the lungs, spreading primarily through the air in droplets as a sufferer sneezes, coughs or talks.
The usual symptoms are a persistent cough, dry at first and with phlegm after four weeks; excessive fatigue; low fever; night sweats; loss of appetite; and weight loss.
The disease can become severe if it is not treated immediately and if the bacterium responsible is hypervirulent. The patient’s susceptibility is also a factor in severity, which is often associated with a deleterious inflammatory response leading to shortness of breath and even pulmonary necrosis. Treatment entails a six-month regimen of antibiotics, which cannot be interrupted or administered irregularly.
In 2022, 7.5 million new and relapse cases of tuberculosis were diagnosed and notified worldwide, the highest number since the World Health Organization (WHO) began global monitoring in 1995. The increase was believed to be largely due to growth in diagnosis and treatment by health services.
Next steps
Initially designed to focus on tuberculosis, the study also tested the role of T cell-specific P2RX7 in mice infected with influenza. The results were similar. “This strongly influenced what I’m doing as I continue to study how damage signals control immune responses,” Santiago-Carvalho said. “In the article, we concluded that CD4+ T cells can be pathogenic. We now want to understand what leads to an increase in this pathogenicity, which we aim to define while determining the underlying mechanisms and potentially extending their analysis to other diseases. If we understand the characteristics of these cells that induce a strong enough response to damage tissue, we may be able to develop alternative therapies.”
Santiago-Carvalho is currently at Mayo Clinic’s Department of Immunology in the United States, working in the laboratory led by Henrique Borges da Silva, penultimate author of the article and lead contact.
Source:
São Paulo Research Foundation (FAPESP)
Journal reference:
Santiago-Carvalho, I., et al. (2023). T cell-specific P2RX7 favors lung parenchymal CD4+ T cell accumulation in response to severe lung infections. Cell Reports. doi.org/10.1016/j.celrep.2023.113448.
#Study #finds #unbalanced #response #worsens #lung #infections