Its different types, the warning signs of its symptoms, and effective ways to prevent it. Gain the knowledge and understanding you need to take control of your health today.
Introduction
Diabetes, a global health concern affecting millions, necessitates an in-depth understanding of effective management. This blog embarks on an extensive exploration of diabetes, unraveling its various types, probing into causative factors, identifying symptoms, detailing management strategies, and shedding light on prevention techniques. Gain the knowledge and understanding you need to take control of your health today.

I. Types of Diabetes
A. Type 1 Diabetes
- Definition and Characteristics
- An autoimmune condition where the immune system attacks pancreatic cells.
- This results in inadequate insulin production, leading to elevated blood sugar levels.
2. Causes and Risk Factors
- Genetic predisposition is often triggered by environmental factors.
- Onset often occurs in childhood or adolescence.
3. Symptoms
- Sudden onset of symptoms such as extreme thirst, frequent urination, and unexplained weight loss.
B. Type 2 Diabetes
- Overview
- Characterized by insulin resistance and inadequate insulin production.
- Develops gradually and is often linked to lifestyle factors.
2. Causes and Risk Factors
- Genetic factors, obesity, sedentary lifestyle, and age.
- Higher prevalence in certain ethnic groups.
- Symptoms
- Gradual onset, fatigue, frequent infections, and blurred vision.
C. Gestational Diabetes
- Occurrence during Pregnancy
- Develops during pregnancy and usually resolves after childbirth.
- Screened during routine prenatal care.
2. Risks and Implications
- Increases the risk of developing type 2 diabetes later in life.
- Can have implications for both the mother and the baby’s health.
II. Understanding the Causes

A. Genetic Factors
- Family History
- Individuals with a family history of diabetes are at a higher risk.
- The interaction between genetics and environment plays a crucial role.
2. Genetic Predisposition
- Ongoing research to identify specific genetic markers.
- Understanding the hereditary aspect aids in early detection.
B. Lifestyle Factors
- Sedentary Lifestyle
- Contributes to insulin resistance.
- Importance of incorporating regular physical activity into daily life.
2. Poor Dietary Choices
- Influence on blood sugar levels.
- Emphasizing the significance of a balanced diet.
3. Obesity and BMI
- Strong correlation between obesity and type 2 diabetes.
- Strategies for weight management as a preventive measure.
C. Insulin Resistance
- Definition and Mechanism
- Cells become less responsive to insulin.
- A central role in the development of type 2 diabetes.
2. Connection to Type 2 Diabetes
- Lifestyle modifications to improve insulin sensitivity.
- Importance of addressing insulin resistance in treatment plans.
III. Recognizing Symptoms

A. Common Symptoms
- Increased Thirst and Hunger
- Polydipsia and polyphagia due to elevated blood sugar levels.
- Recognizing these signs for early detection.
- Frequent Urination
- Polyuria is a result of the kidneys attempting to remove excess glucose.
- Impact on daily life and potential complications.
- Fatigue and Irritability
- Depletion of energy due to inadequate glucose utilization.
- Mental health considerations and coping strategies.
- Unexplained Weight Loss
- Sign of uncontrolled diabetes, often seen in type 1.
- Immediate medical evaluation is crucial.
B. Complications of Untreated Diabetes

- Cardiovascular Issues
- Increased risk of heart disease and stroke.
- Managing cardiovascular health as part of diabetes care.
- Nerve Damage
- Neuropathy and its symptoms.
- Importance of foot care and monitoring nerve health.
- Kidney Problems
- Nephropathy and implications.
- Regular monitoring of kidney function.
- Vision Impairment
- Diabetic retinopathy and its progression.
- Regular eye examinations to prevent vision loss.
IV. Management Strategies

A. Medications
- Kidney Problems
- Types of insulin and their applications.
- Individualized treatment plans based on patient needs.
- Oral Medications
- Medications for type 2 diabetes.
- Managing side effects and potential complications.
B. Lifestyle Modifications

- Healthy Diet Choices
- Emphasis on a balanced diet.
- Understanding the glycemic index and carbohydrate counting.
- Regular Physical Activity
- Exercise’s impact on blood sugar levels.
- Tailoring exercise plans to individual fitness levels.
- Weight Management
- Correlation between weight and diabetes.
- Sustainable approaches to weight loss.
C. Monitoring Blood Sugar Levels
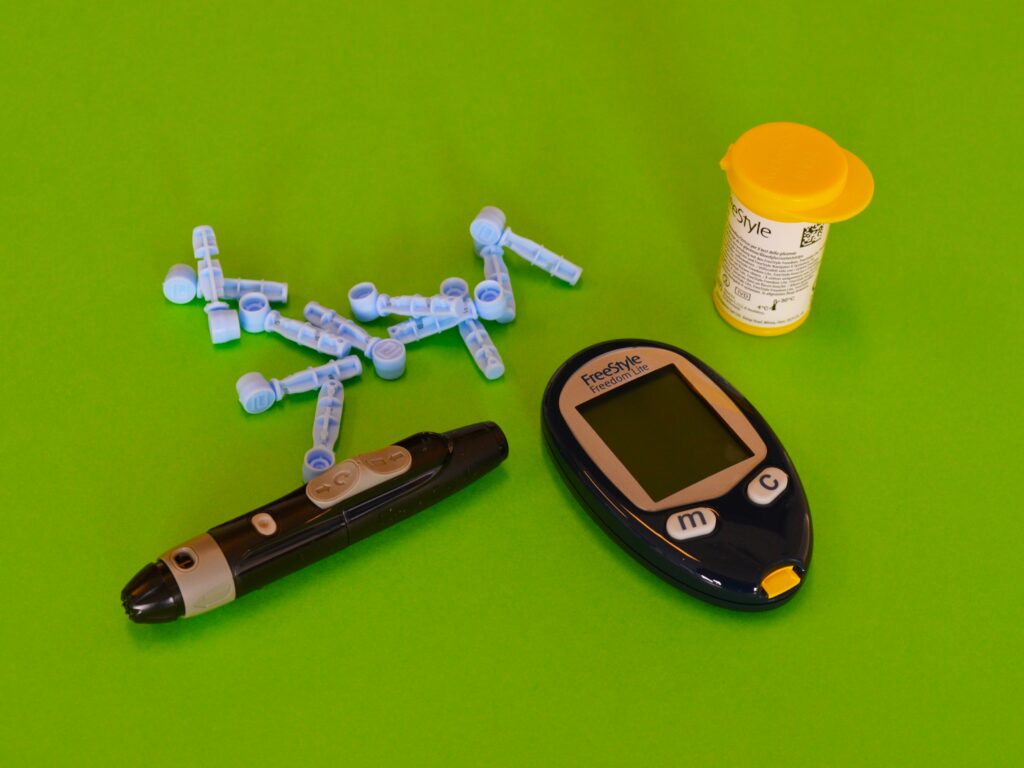
- Importance of Regular Monitoring
- Self-monitoring and its benefits.
- Introduction of Continuous Glucose Monitoring (CGM) systems.
- Using Glucose Meters
- Correct usage and interpretation of results.
- Analyzing patterns and making necessary adjustments.
V. Prevention Techniques

A. Healthy Eating Habits
- Balanced Diet
- Incorporating whole foods.
- Meal planning and portion control as preventive measures.
- Portion Control
- Managing portion sizes to avoid overeating.
- Stabilizing blood sugar through mindful eating.
B. Regular Exercise
- Importance of Physical Activity
- Exercise as a preventive measure.
- Tailoring exercises to individual fitness levels.
- Types of Exercises for Diabetes Prevention
- Incorporating aerobic exercises and resistance training.
- Consistency and finding enjoyable physical activities.
C. Routine Check-ups
- Regular Blood Sugar Tests
- Establishing a routine for monitoring blood sugar levels.
- Adjusting treatment plans based on test results.
- Health Screenings
- Comprehensive health assessments for early detection.
- Monitoring for diabetes-related complications.
VI. Living with Diabetes

A. Coping Strategies
- Emotional Support
- Acknowledging the impact of diabetes on mental health.
- Seeking professional counseling and peer support.
- Diabetes Education Programs
- Empowering individuals with knowledge.
- Continuous learning and adapting to new information.
B. Creating a Supportive Environment
- Family and Friends
- The pivotal role of a strong support system.
- Educating loved ones about diabetes management.
- Workplace Support
- Navigating diabetes in the workplace.
- Effective communication and accommodation strategies.
Conclusion
In conclusion, diabetes is a complex condition that demands a holistic approach to management and prevention. By unraveling its intricacies, individuals can make informed choices, incorporating medication, lifestyle modifications, and preventive measures into their daily lives. Understanding the impact of genetics, lifestyle factors, and the importance of regular monitoring empowers individuals to navigate their diabetes journey with resilience, leading to a healthier and more fulfilling life. Regular check-ups, a supportive environment, and continuous education form the pillars of successful diabetes management. Through comprehensive efforts, individuals can not only manage diabetes effectively but also reduce its impact on their overall health and well-being.


